There are no beds. The sick and the dying are left outside while stressed-out healthcare professionals work round the clock to help them. Elective procedures are cancelled, previously closed beds are reopened. It is a surprise. The ensuing media storm assures us the situation is unacceptable. The doctors’ representative, the nurses’ representative, the union representative, the patients’ representative, the minister and the technocrats who run the system are all over the airwaves, because the situation is unacceptable. The solution is more money. Much more money. Money and time. Because change will take place, but only over a number of years. And change must happen. Because this is unacceptable
This is the narrative in the second week of January for almost every year since 1978. Nineteen seventy-eight!
I searched the front pages of every major newspaper in the country last week, and guess what? It’s the same story. You might as well get 2018’s copy ready now. Same exact story, often with identikit quotes from many of the same people, each one gravely shaking their head and earnestly committing to solving the problem of our ongoing national health emergency.
Here’s a thought: it’s not an emergency if the situation has persisted longer than 25 per cent of the population of the country has been alive. It’s just how it is. The papers merely report the annual failure to deal with a predictable surge in demand.
Why is this happening every year?
The answer is actually very simple. The ‘emergency’ is caused by sustained under investment in capital – like primary care centres and hospitals – combined with a rapidly aging population who will demand more of these services over time. The result is overcrowding and poor patient outcomes. The ‘emergency’ will get worse over time. As we will see, the system will need massive investment in the coming ten years just to stand still. This should not be news to you if you’ve been reading Susan Mitchell’s coverage in this newspaper.
To understand why we’re in this situation of repeated ‘emergency’, we must remember where our health system comes from — charities and local authorities in the 19th and 20th centuries.
The Department of Health was formed in 1947, and enshrined our two-tier system by deciding in 1949 that true universal health insurance was unaffordable. It is important to remember the National Health Service model adopted by Britain after the Beveridge Report was fiercely resisted in Ireland by the medical profession, the Catholic Church and the Department of Finance. Their reasons for objecting nearly 70 years ago are as obvious as they were shortsighted.
There was no national approach to health care until 1970, when eight regional health boards were created, removing responsibility for healthcare from local authorities. (The eight would morph into 11 as Dublin grew). The result is a strange mix of of heavily-subsidised services, state and private health insurance, beginning with the VHI in 1957, with payment for services at most points of use for services such as dentistry and GP visits. Ruth Barrington’s excellent book Health, Medicine and Politics in Ireland, 1900-70 details the development of the health service very well.
The long and the short of it is that our services developed in a patchwork, and as largely local entities. The result was deep inefficiency and rent-seeking as a cadre of small charities and more than 40 semi-state agencies grew up to address significant issues. Centralisation of these services only began in 2005 in earnest with the creation of the Health Service Executive. Someone retiring from the HSE at 65 today would have been through five or six reorganisations, without altering the fundamental nature of our system. It doesn’t matter when St Vincent’s Hospital is funded by a local authority, a council, a regional health board, a national health service executive, or as part of some larger entity. It is still largely the same building built in 1970 and paid for through a big grant to the nuns who own it by the state.
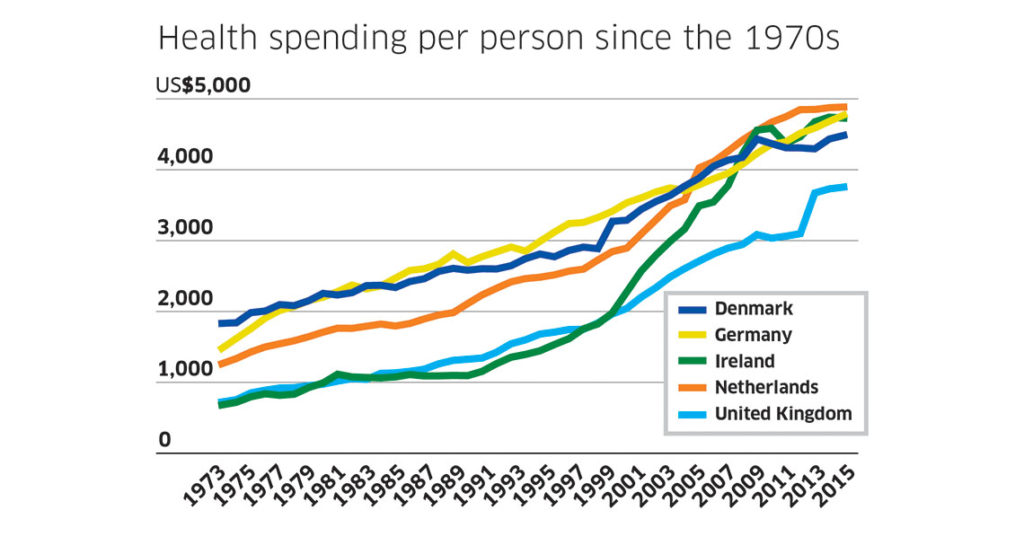
This weird, hotchpotch health system development would not have been much of a problem if, around 1960 or so, investment had begun to modernise the health system to bring it into line with health services around the world. Comparing Ireland to, say, Britain, Denmark, Germany and the Netherlands, from 1970 to today, we see that Ireland and Britain spent the least per person until the late 1990s. Unlike Britain, we don’t have the efficiencies you get with a single universal system. So not only were we spending less, we were spending what we had in an inefficient way.
When you correct for inflation and currency differences, you can see that in (say) 1978, Ireland spent $925 per person on health. Britain spent $953 per person. Germany spent $2,154 per person on health, Denmark spent $2,152 per person, the Netherlands spent $1,645 per person. Some of this spending is to pay doctors and nurses, some for medicines and bandages, and some for capital spending on hospitals and ambulances. Some of this spending is cumulative — tomorrow’s spending builds on today’s.
The fact that Germany, Denmark, and the Netherlands spent nearly double the amount per person we have for 40 or more years has a huge effect on the health system they see today. Note also that the Irish data probably overestimates how much we spend on ‘health’. Because of the weird way our system evolved from the 19th century, a lot of the stuff our health system does would be classified as social protection spending in other countries. Nonetheless the trend is clear: we see a sustained lack of investment over decades, and a system much less efficient than Britain’s one-tier, national universal health system, so even when the money came pouring in in the 1990s, bringing Irish health spending per person up to $4,730 in 2015, while Britain spends $3,756 per person.
This sustained investment has real consequences. For example, in Germany today, there is a major scandal in their health system. Like us, they have a flu outbreak. Patients must wait three hours to be seen. Three hours. That’s a scandal in Germany in 2017.
Another way to look at the practical effects of underinvestment: in 2015 the average waiting time to be seen on a list for common procedures such as coronary angioplasty, cataract surgery, hip and knee replacement, and the like, is 183 days in Ireland. Germany’s average waiting time has climbed to 29 days, and there that is considered a scandal for which the relevant minister must have their feet held to the fire.
Any Irish health minister who delivered 29-day average waits for cataracts and coronary bypasses would be beatified before death and treated better than Jack Charlton everywhere they went. That’s the real measure of underinvestment: lack of capacity leading to much poorer outcomes for citizens.
In terms of systems, Ireland’s hotchpotch is the worst of all worlds. Sustained underinvestment in the public system created large demands for private provision by the middle classes, which the market met. Once demographic pressures built up and the public system was unable to meet even the most basic of demands, the solution has been to purchase more health services in the private sector using public money, or to purchase health services outside the state.
You have consultants paid by the state using public resources for private work, and all sorts of other weird effects. Ultimately the only solution is a properly resourced one-tier health system. This would be fiercely resisted as it would make some people much poorer, and would be vastly, vastly more expensive for the public purse in the short to medium term.
We must be fair to the 105,000 people working in the HSE. There have been very large changes, both within the system and the funding envelopes they were given. The number of hospital beds available for acute purposes has dropped by 13.5 per cent since 2006 to 10,473, but the number of beds for day cases has risen by almost 43 per cent to 2,026. There has been an increase of 55 per cent in the number of day cases in hospital since 2006. In 2015 the HSE saw over 1 million day cases. This is a result of the bizarre and under-studied interaction of austerity policies and medical technology.
The structure of the system is why, despite large levels of spending since the late 1990s, and having one of the most expensive health systems in the OECD, Ireland lags much of our comparator group in terms of health outcomes. It is the structure that needs to change.
No structural change without some capital spending
Why haven’t we seen structural changes to bring our waiting times down to the German or Dutch levels? Remember that we have gone broke as a country three times since independence: the 1950s, the 1980s and the late 2000s. The result of these periods when there wasn’t enough money to run the state is that large capital programmes like modernising hospitals, roads, and schools just don’t get done. It’s easy to see why. The public will go mad if social welfare payments or child benefit or carer’s allowances get cut, and rightly so. Few mourn the loss of a hospital wing that was never there in the first place.
Since independence, the rule has been that, when times are tough, cut back on capital investment. The result is a sustained under investment in health services.
We have to place the health services of this country in the perspective of its recent fiscal history. As always, the data tell the story better than I could. In the 1970s and 1980s, thanks to our economic fortunes, capital spending was essentially non-existent in our health service. The same hospitals and care centres built in the 1870s, as well as the 1930s and 1940s as sanatoria for tuberculosis and asylums treated a population of roughly 3.4 million people in 1980.
This regionalised system came under strain as austerity bit in the mid-1980s, and again in the late-1990s with a booming population pushing past 4 million to today’s 4.76 million people. (Look at the graph which measures only capital spending.)
You can clearly see a large increase in expenditure during the 1990s and early 2000s and a collapse in capital expenditure during the recent crisis. The government’s capital plan will bring us back to the 2008 level of capital spending by 2020 or so, when we will spend €6 billion on health alone. Much of this spend is tied up in one project — the national children’s hospital.
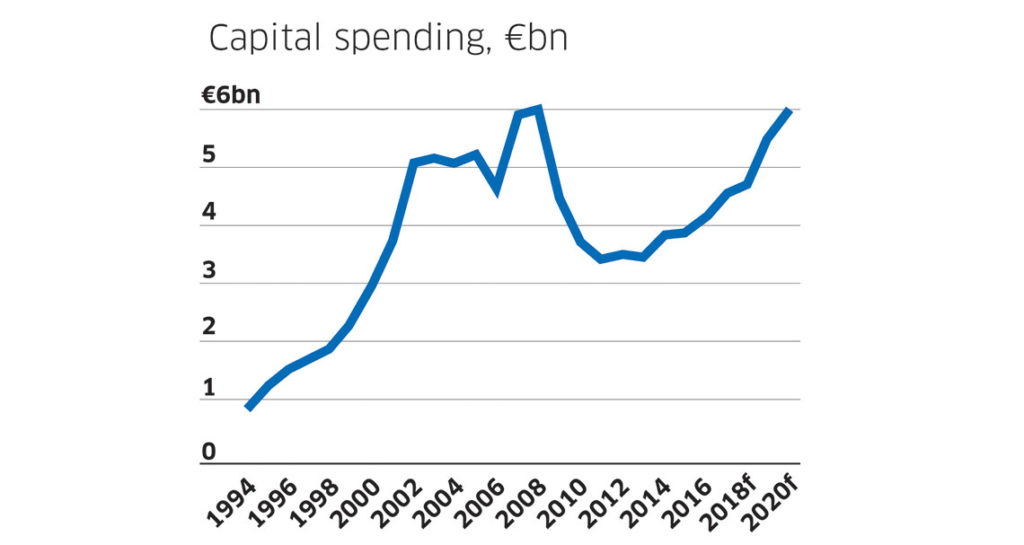
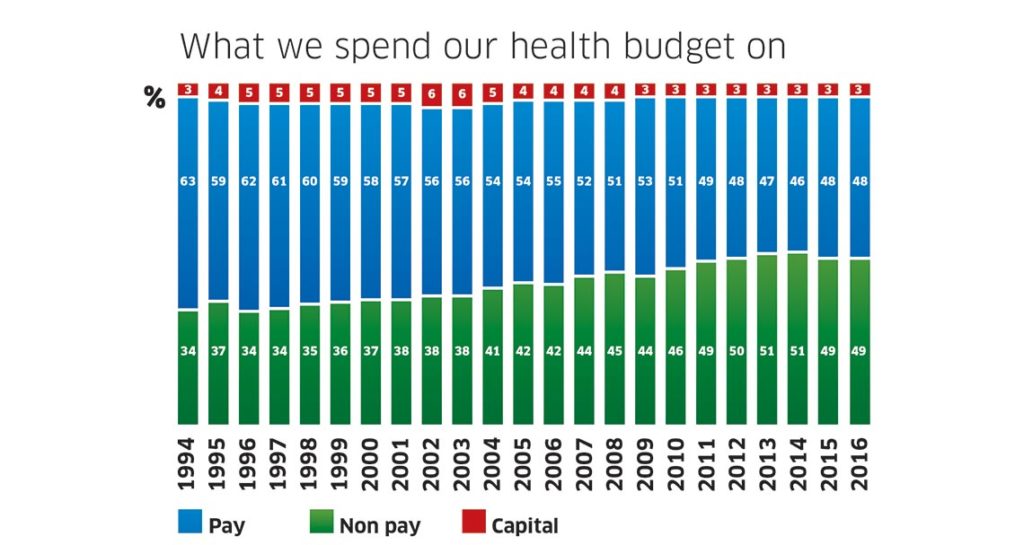
It’s worth thinking about capital spending as a proportion of the total spend on health. Even as the total health budget boomed from €3 billion in 1994 to €13.5 billion in 2016, the proportion spent on capital was tiny. Never in more than 20 years has capital spending in health been above 6 per cent of the total spend, and it was only at 6 per cent twice in 22 years.
When there were years of plenty, much of the increase went on pay. An example: over the period from 1996 to 2001, what we might call the Celtic Tiger years, 65 per cent of all increases were on pay alone, while the workforce increased by 18 per cent in that period.
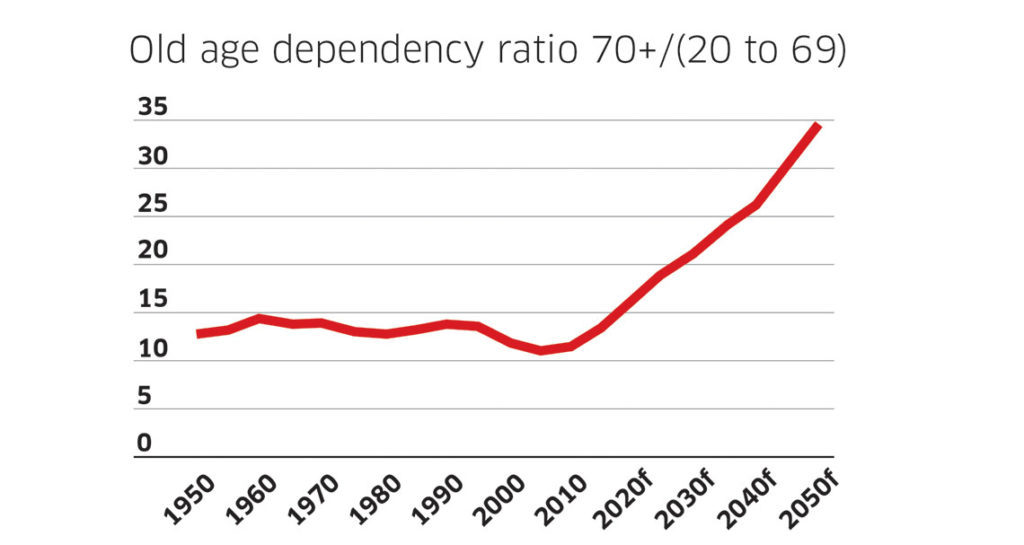
I mentioned at the start that things would get worse for our health service. The next chart shows the old-age dependency ratio, which measures the number of people aged 70 and over divided by the number of people aged 20 to 69. I include its projection out to 2050. The old age dependency rate triples, meaning there will be far fewer young people relative to older people, and so the relative burden of paying for their care will increase. The big change here is just how many older people there will be by 2030.
If talk of 2030 and 2050 leaves you cold, think about this. By 2021 there will be an extra 136,000 people aged over 85 than today. Each of these citizens will need more healthcare than other citizens, and many will need much more. Another way to think about this: we’ll add roughly 20,000 more people aged over 75 every year for the next 20 years. Unless we decide to stop funding care for our elderly, these people will need hospitals, primary care centres, occupational therapists and the full suite of increasingly expensive medical technologies.
The upshot? More people will need to use facilities which haven’t been improved upon for decades within an imperfect system that still uses sticky labels to do much of its work. The result is a seasonal crisis every year.
We shouldn’t sell our health system short. It is a deeply flawed system that shows the long-term damage that poor policy decisions can have. If in the 1940s we ignored the doctors, the priest and the civil servants, and followed Britain’s NHS model, our outcomes for our patients would surely be better today. If we had increased and ring-fenced capital spending to the level our European cousins were spending since the 1970s, our outcomes for our patients would surely be better. But those things didn’t happen. We are stuck with the system we have, and that system is going to come under intense strain over the coming decades.
Ireland’s system of health accounts counts government-funded services, household out-of-pocket payments for medicines and other professional fees, as well as private health insurance funding. It reports that we spent around €20 billion in 2014. Of that €20 billion, only €894 million was directly measured by the CSO as capital spending. Without a large increase in capital spending, there is no hope of changing the health system Ireland’s citizens currently have. Ireland spends proportionately more on health than any EU country and more than any other rich country except for the United States.
It’s the system, stupid. It is not an accident that Ireland ranks in the bottom third internationally in many of the measures of health performance the OECD uses. It is not an accident we have some of the most expensive hospitals in the OECD. It is not an accident Ireland’s spending on prescribed medicines is the second highest in the EU. It is not an accident that we rank in the bottom third of countries for the number of doctors and hospital beds, adult obesity, alcohol consumption, and female life expectancy at age 65.
It is not an accident we produce the highest number of medical graduates but also rank fourth for the number of foreign-trained doctors. It is not an accident Ireland has more nurses than most of the OECD but still manages to have a nursing shortage. These are the outcomes of decades of short-term thinking.
It’s not like the HSE is unaware of any of what I’ve written. Just read the HSE’s National Service Plan for 2017. The biggest risks to delivering the service plan? Controlling pay and staff numbers while a larger number of people than ever before seek to access services as the population grows.
The Future of Healthcare committee within the Oireachtas is due to publish its report soon. The solution to the question of healthcare provision in the 2020s is not simply more money. Ireland has tripled its health spending, and already spends a comparable amount to countries such as Germany and the Netherlands. As I’ve shown, much of these increases came as pay for existing and new workers, rather than expansions in service provision. The solution is a single, unified system, with a smaller number of excellent hospitals and a larger number of primary care centres. Nurses and doctors we educate here leave in droves because they don’t want to work within the system we’ve built over decades.
I once gave a grand rounds lecture to doctors in University Hospital, Limerick, which is now part of the University of Limerick.
(This hospital had 90 per cent of the Midwest’s ambulances parked outside it last week. Its A&E was too full to admit them. Think about that).
During the lecture, I showed the doctors the figures on employment in the health service, which had shrunk from 120,000 in 2008 to 100,000 in 2014. I presented them with a thought experiment: if I handed them the money for the 20,000 extra people, to return them to their 2008 heights, what types of worker would they like to hire?
The entire room agreed they wouldn’t spend the cash on people at all. They would spend it on new systems, particularly better ICT and analytics. I asked the junior doctors how many were thinking of leaving once their training was complete. They all put their hands up.
Pay alone won’t bring them back. Irish hospital consultants already earn far more than their British and German counterparts. But they also work far, far harder, in a very difficult environment. They might work far harder for themselves, but there’s no doubt they work hard. It’s easy to have a pop at someone on €220,000 plus a year. It’s much, much harder to suggest changes that would see more consultants working less but working smarter, with better data and analytics on patients and their needs and a unified system-level approach.
A system-level approach
That approach means tricky governance questions must get solved. Bunfights over which order of nuns own which hospital wing must go. An example: transfer of ownership of St Michael’s hospital to the Religious Sisters of Charity took place in 2001 in exchange for the Children’s Hospital, Temple Street. Why? Nuns shouldn’t own hospitals funded 100 per cent by the state. (I’m not taking a pop at nuns. Economists from the University of Limerick shouldn’t own hospitals either.) The state should own hospitals funded 100 per cent by the state. A general rule should be that if the state funds more than 60 per cent of your service, it’s properly considered a part of the state.
That approach means not everyone can have the Mater Private in their front garden. That approach means some people must get redeployed or retrained or fired.
That approach means we as individuals will need to pay more for our own care as we get older, either via insurance markets or through increased taxes.
That approach means either effectively nationalising large parts of the private healthcare system to rectify the mistake we made in the 1940s by not building an NHS when we had the chance or privatising most of what’s there to make it drastically more efficient. I favour nationalisation.
That approach means building new primary care centres and new hospitals to cope with an older population, systematically over investing in a system we’ve starved of capital since before most of us were born.
That approach means lots and lots of powerful people and interest groups will be told ‘no’. Because this is unacceptable.
The alternative is to get the stories of overcrowding and patients in distress for 2018, 2019, 2020, and 2021 ready now, and to understand that if we don’t change the system, society is deciding that stories of overcrowding and patients in distress are acceptable.
